Smart Tech Infrastructure for Scaling Affordable Cannabis Coverage Nationwide
Summary
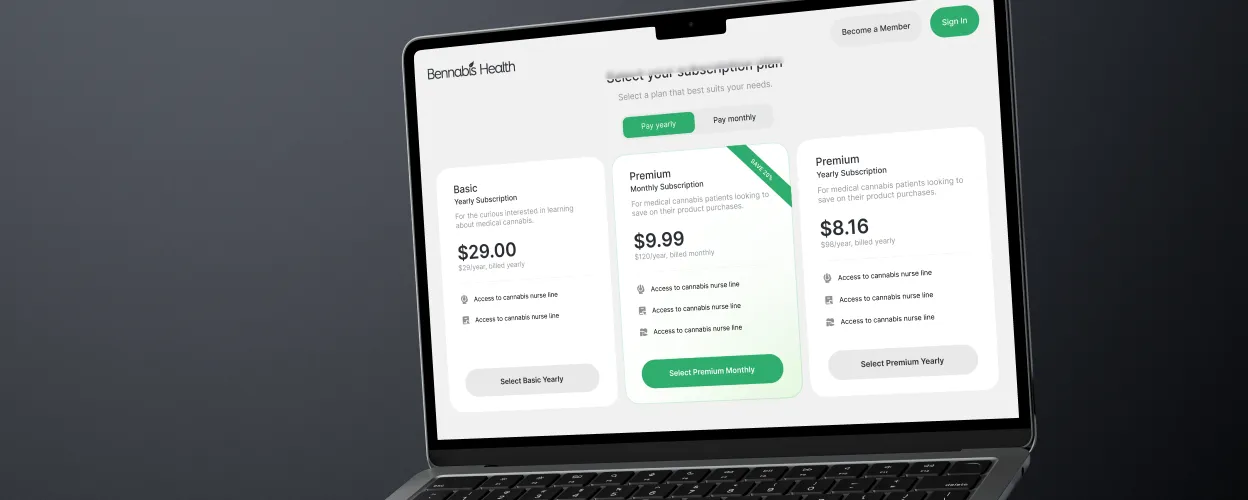
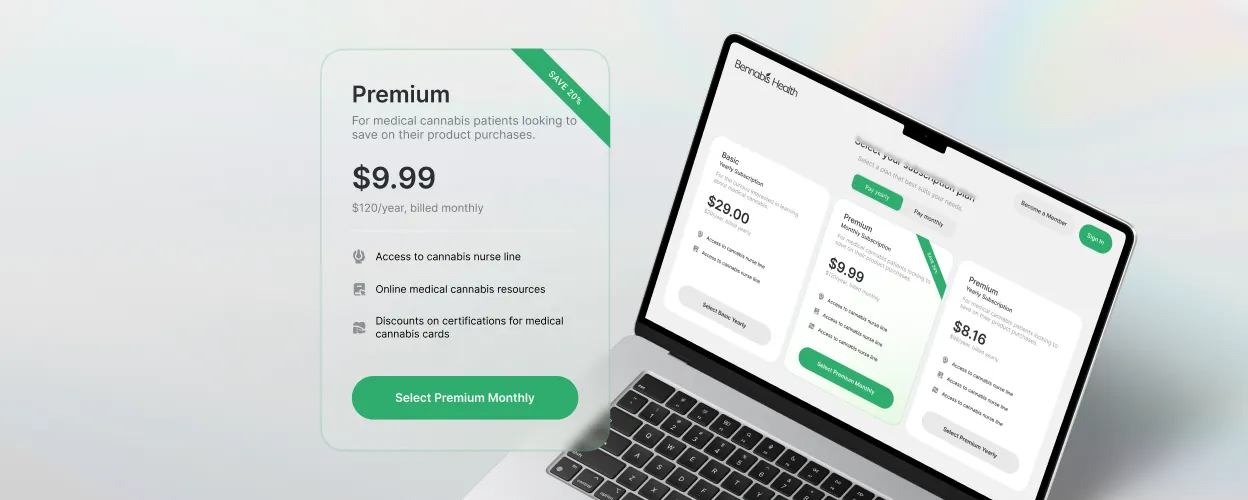
Bennabis Health set out to expand access to affordable medical cannabis by offering both individual and employer-sponsored plans, but their original platform wasn’t built to support group benefit workflows, eligibility data, or scalable admin tools. Momentum helped stabilize the system, enable group plan functionality, and prepare the business for long-term growth.



Setting the scene
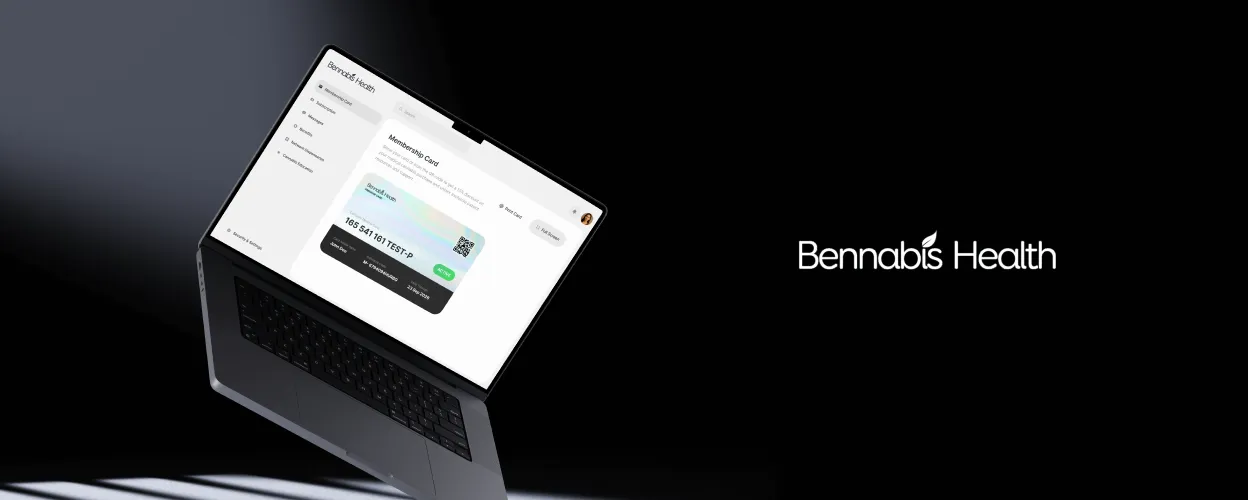
Bennabis Health’s mission to make medical cannabis accessible and affordable began with a strong focus on individual plans. Members could save on their prescriptions through a network of dispensaries across the U.S., supported by an intuitive platform that streamlined access.
But Bennabis wanted to do more—they envisioned a future where employers could provide this benefit to employees, creating group health plans that offered savings and support to entire organizations.
Months after successfully launching individual plans, Bennabis identified the need to expand their platform’s capabilities to serve group plans. However, the system wasn’t equipped to handle the complexity of organizational sponsorships, eligibility file management, or the scalability required for this transformation. That’s where we came in—partnering with Bennabis to create a platform that could stabilize their existing operations and unlock future growth.
What we were up against
How do you build a platform that supports individual plans today and group health plans tomorrow without disrupting either?
The road to enabling group health plans was marked by two distinct phases of challenges. The first phase focused on stabilizing Bennabis’s existing platform to support individual memberships effectively. Without this foundational work, scaling would have been impossible.
Once stability was achieved, the second phase introduced a new layer of complexity: adapting the platform to manage group plans. This required implementing features like organizational sponsorships, eligibility file uploads, and seamless onboarding for employees. Here’s what had to be addressed:
Eligibility File Uploads at Scale
We introduced automated validation and batch processing to ensure large eligibility files could be uploaded without errors or service interruptions.
Secure Handling of Sensitive Data
We implemented robust encryption protocols and data protection standards to manage Social Security Numbers (SSNs) and other personal data without compromising compliance.
Seamless Continuity for Existing Members
All changes were delivered without downtime. Careful rollout planning and rigorous testing ensured uninterrupted access for current users.
A Platform Architecture Built for Growth
To support future features and new markets, we restructured the system around modular components making it easier to scale without technical debt.
.webp)
Four things that had to work perfectly
Before we could build or scale anything, we had to be crystal clear on what success looked like. These four criteria shaped every technical and design decision ensuring the platform would deliver immediate value and remain future-ready.
Seamless integration with existing flows
Group plans needed to fit cleanly into the current Bennabis experience without introducing friction for individual (B2C) users or disrupting live services.
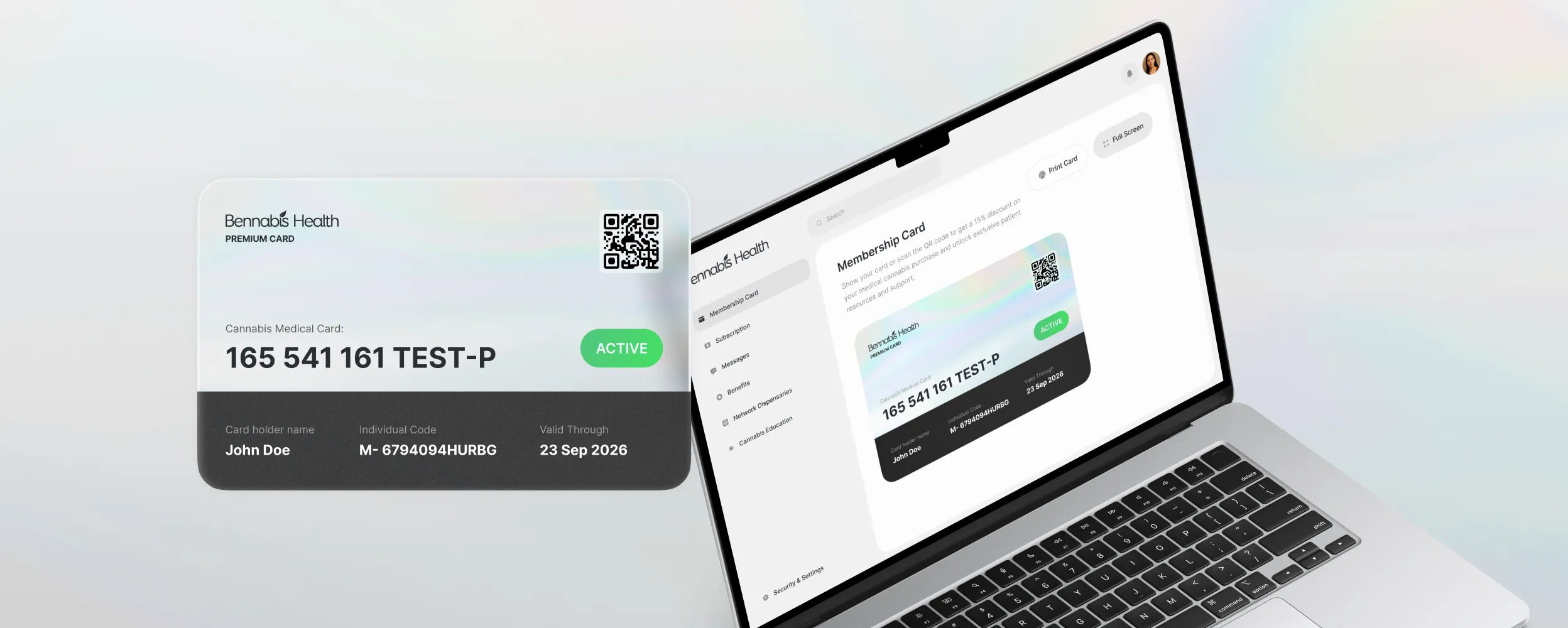
Clear enrollment paths for all members
Both individual users and employees joining through group plans had to access, enroll, and manage their benefits without confusion regardless of their entry point.
Effective admin management tools
Admins and benefits managers needed the ability to oversee eligibility, onboard new members, and manage billing without time-consuming manual steps.
Secure processing of eligibility data at scale
Eligibility data had to be processed in bulk, encrypted end-to-end, and aligned with compliance standards ensuring stability from day one and growth beyond it.
Building the strategy
We designed a phased strategy to ensure immediate improvements while laying the groundwork for long-term scalability. Each phase focused on distinct needs and outcomes, driven by close collaboration with Bennabis.
Stabilizing the Foundation
We started by rebuilding the backend using Laravel and redesigning the React-based frontend into modular applications. This improved overall stability, enabled easier maintenance, and set the groundwork for future scalability. We also migrated to high-performance U.S.-based servers to boost speed and reliability.
Enabling Group Plan Functionality
With a stable core in place, we built new features to support group health plans. These included secure eligibility file uploads, automated member validation, and workflows that made onboarding seamless for thousands of employees.
Preparing for Scalable Growth
The upgraded architecture supports modular expansion, allowing Bennabis to adapt the platform for new markets, products, and plan types. This future-ready setup ensures the business can scale without rework or disruption.
How we got it done
Before writing a single line of code, we worked closely with the Bennabis team to align on business priorities and define the scope of the next product iteration. We started with deep-dive sessions focused on their updated business model and goals for expanding into employer-sponsored plans.
This led to a two-week workshop phase, where we mapped the current platform as it stood and how it would need to evolve to support group benefits. We broke down the platform by user role and identified the minimal, clearest paths needed to:
- Invite and onboard group members
- Manage subscriptions
- Administer eligibility at scale
From there, we phased the scope to deliver the highest-impact features first, ensuring we could build a group benefits MVP within two months without overengineering or overspending. Wireframes were created in parallel to visualize new flows, align expectations, and accelerate development once the plan was approved.
The tech behind the magic
Behind the scenes, Bennabis needed a platform architecture that could handle complex data flows, scale across user types, and integrate seamlessly with their existing operations. Every piece of the tech stack was selected to balance performance, security, and flexibility, making the system easy to manage today and ready to grow tomorrow.
Backend
Laravel (PHP) for scalable architecture
Frontend
Modular React applications for members, sponsors, and admins
Database
MySQL/MariaDB for reliable data management
Task Management
Redis for handling intensive background processes
Payment Processing
Authorize.net for compliant, industry-specific transactions
Hosting
High-performance U.S.-based servers

What we achieved together
Bennabis Health’s reimagined platform now supports both individuals and employer-sponsored members, opening the door to sustainable growth.
With automated workflows for eligibility management, onboarding, and reporting, administrative burden has been significantly reduced. The internal team is free to focus on strategic initiatives while the platform continues to deliver a reliable, intuitive experience for users.
Whether members join through individual plans or employer partnerships, they benefit from a smooth onboarding process and a personalized portal to manage their coverage. The result: better access, stronger engagement, and a platform ready to scale.
"Momentum’s workshops were a game-changer for us. Their team took the time to deeply understand our mission and challenges, asking the right questions and aligning their solutions with our vision. It felt less like hiring a vendor and more like gaining a partner who truly cares about our success."

From secure eligibility processing to scalable architecture, Bennabis now operates on a platform designed for both flexibility and scale. With group plans live and future expansion in reach, they’re equipped to serve more members, more efficiently without compromising performance or trust.
You can learn more about their work at Bennabis Health.

Ready to turn a healthcare vision into a scalable digital product?
Read more case studies

Fewer forms, happier patients: How Villa Medica leveraged AI to boost patient outcomes
.avif)
Instant lab results: How Labplus and Momentum cut processing time from days to minutes













.avif)

.avif)


.webp)



.png)

.png)
.avif)